Effectiveness of multisectoral collaboration in implementation of One Health Approach for control of zoonoses in Kisumu, Kenya
Abstract
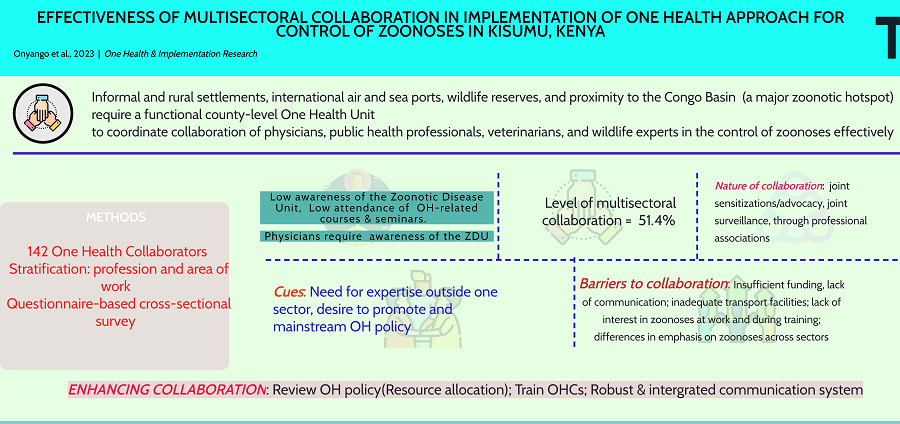
Aim: One health (OH) integrates the efforts of multiple disciplines working locally, nationally, and globally to achieve optimal health for people, animals, and the environment. Changing interactions between people, animals, plants, and the environment have resulted in the growth and expansion of human populations into new geographic areas. The proximity to domestic and wild animals, climate changes, and land use distort the environment leading to opportunities for the amplification of zoonoses. Implementing the OH approach at the national, local, and project level remains limited due to the lack of practical and tested operational methods for implementation and evaluation. In Kenya, the OH approach is spearheaded by the Zoonotic Disease Unit (ZDU). This study assessed the proportion of partners collaborating for OH, the methods, and the factors affecting multisectoral collaboration to confirm its effectiveness in controlling zoonoses in Kisumu County.
Methods: A cross-sectional descriptive study design was used to generate information regarding the effectiveness of multisectoral collaboration in implementing the OH approach in the control of zoonoses. Descriptive statistics determined and assessed the nature, extent, and factors that affected multisectoral collaboration.
Results: Multisectoral collaboration to control zoonoses in Kisumu was limited and driven mainly by public health officers (PHOs). Collaboration was enhanced through joint sensitizations and notifications whenever a zoonosis was suspected. The need for expertise outside one sector, the desire to promote OH, and the requirement to mainstream OH as a government policy prompted multisectoral collaboration.
Conclusion: Multisectoral collaboration needed to be improved owing to a deficient OH policy hence the need for review to optimize the limited funding for training and infrastructure development, addressing staffing requirements, and setting up a robust information management system for data sharing.
Keywords
INTRODUCTION
OH is an integrated, unifying approach that sustainably balances and optimizes the health of people, animals, and ecosystems[1,2]. The approach recognizes the intricate connection between people's health and that of animals, including their shared environment[3]. It aims to design and implement programs, policies, legislation, and research in which multiple sectors communicate and work together to achieve better health outcomes[4].
The encroachment into new geographic areas leads to changes in climate and land use, creating the risk of environmental disruption that develop opportunities for outbreaks and epidemics[3]. These pathogens can now spread quickly across borders and around the globe because of the movement of people, animals, and their products due to increased international travel and trade. According to the available literature, approximately 60% of all human infectious diseases currently recognized and about 75% of emerging infectious diseases that have affected humankind over the past three decades are zoonoses[5]. Zoonoses are emerging and reemerging almost every year, mainly driven by the increasing global population, aging, travel, urbanization, and climate change, which favor pathogen emergence, evolution, and spread[6]
Zoonoses have caused global societal and economic impacts related to unexpected illnesses and deaths, including interference with travel, business, and everyday life activities[7]. Some of the emergent diseases include Severe Acute Respiratory Syndrome (SARS), West Nile fever, avian influenza, hantavirus disease, Rift Valley fever (RVF), Marburg virus disease, influenza A, Middle East Respiratory Syndrome (MERS), Ebola Virus Disease, Zika fever, and recently, COVID-19[6-9]. Zoonotic pathogens crossing over into human hosts may cause endemic health burdens. These diseases are prevalent among communities in low-income settings, characterized by high population growth rates, animal husbandry, and lack of capacity in a skilled workforce to manage outbreaks[9,10].
Recognizing the threat of emerging and reemerging zoonoses globally led to advocacy for adopting OH approaches to strengthen monitoring and response to zoonotic disease risks through multisectoral and transdisciplinary collaboration[11,12]. Implementing the OH approaches has been attempted with varying degrees of success and challenges[13]. Implementation of OH approaches at country, local, and project levels remain limited due to the great variety of potential risk scenarios and a need for tested methods for implementation and evaluation[12].
In Europe, the OH approach focused mainly on antimicrobial resistance, leaving zoonoses to veterinary services[14]. In Africa, the OH approach was spearheaded by a network of universities, mainly in central, western, and eastern Africa. They collaborated in building academic partnerships for OH in public health and veterinary medicine schools[15]. In Kenya, the OH approach commenced in 2006 following the establishment of a multisectoral committee to coordinate preparedness efforts to prevent the spread of highly pathogenic avian influenza[10]. The initiative was immediately tested by RVF outbreak, providing lessons concerning collaboration between health and veterinary services[16]. The partnership led to the creation of a Zoonotic Disease Unit (ZDU) in 2012 to coordinate OH activities in Kenya through collaboration between the ministries responsible for health and livestock via policy creation, advocacy, communication, and leadership to strengthen surveillance, detection, prevention, and control of zoonoses in humans and animals, including conducting research and training at the human-animal and ecosystem interfaces[15].
The benefits of research in OH approach include global improvement of animal and human health through multisectoral collaboration, addressing critical needs, and developing centers of excellence for education and training. This study aimed to assess the extent, nature, and factors that affect multisectoral collaboration for One Health approach for controlling zoonoses in Kisumu County.
METHODS
Study area
Kisumu County is approximately 2,576.5 sq. km, with 567 km2 covered by water. The county’s population was 1,155,574, with a density of 554 per sq. Km. Livestock population for cattle, sheep, goats, donkeys, and poultry was 249360, 247,652, 745,500, 3,490, and 3,378,493, respectively[17]. The area has a city with informal and rural settlements and international air and sea ports. It hosts wildlife reserves and a sanctuary near the Congo Basin, a major zoonotic hotspot. However, there needed to be a functional county-level One Health Unit.
Target population
The study targeted physicians, public health professionals (PHOs), veterinarians, veterinary paraprofessionals (VPPs), and wildlife professionals (ecologists and wildlife VPPs) within Kisumu County, as proposed in the One Health Strategic Plan for the Prevention and Control of Zoonotic Diseases in Kenya[18].
Study design
The study adopted a descriptive cross-sectional approach involving both quantitative and qualitative data.
Sample size determination
The minimum sample required was estimated using the Cochran formula[19].
n = Z2pq/e2
Where: n = minimum sample required; e = margin of error (5%), P = proportion of one health collaborators (OHC) with knowledge of zoonoses (unknown; set at 50%), q is 1 – P, Z = standard normal deviate at 95%CI (1.96). The population of OHCs in Kisumu was established to be 193; therefore, using the finite population correction factor[19], the adjusted sample size was (n0) = n × N/n + (N – 1) was 129, but the researcher increased it to 142 participants to accommodate non-responses.
Sampling procedure
The 193 OHCs from the county directorates of health and veterinary services and Kenya wildlife service Lake Region constituted the primary unit for sampling purposes. They were stratified in terms of profession and sub-county. The diverse nature of the target population necessitated the use of a stratified sampling technique to proportionately recruit 142 OHC from a sampling frame established from the primary unit. Participants were, after that, conveniently selected depending on their availability at their workstations and willingness to participate.
Inclusion criteria
Only physicians, public health professionals, veterinarians, veterinary paraprofessionals employed by the County government of Kisumu, and wildlife officers (veterinarians and ecologists) working in the national government but stationed within Kisumu County, present at their workstations and willing to participate were included.
Data collection and analysis
A pretested, semi-structured, self-administered questionnaire was provided to the respondents at their workplaces. The Interviewer remained nearby for any clarification. Data were cleaned, validated manually, and analyzed using Statistical Package for Social Sciences (SPSS IBM) version 26. Nature, extent, and factors that affected collaboration were determined and assessed using descriptive statistics (frequencies, percentages, averages, mean and standard deviation). Chi-Square was used to test the association between categorical variables with the P-value set at a 0.05 significant level. Collaboration was considered adequate at 70%.
Study variables
The independent variables were the extent of multisectoral collaboration among the One Health partners, with particular emphasis on which sector initiates the collaboration, the nature of multisectoral collaboration, and the factors that affect multisectoral collaboration. The intervening variables were government policies related to staff employment, deployment and retention in the various sectors, and the occurrence of natural disasters such as extremes of weather, epidemics, and pandemics. The dependent variable was the control of zoonoses.
RESULTS
Characteristics of the study participants
A total of 142 respondents participated in the study, of which (70.4%, n = 100) were below 45 years, with the majority from the human health sector and most having bachelor-level education [Table 1]. A majority needed to be made aware of the existence of the ZDU [Table 2]. Other than their primary pre-service course, most respondents did not attend any one health-related course [Table 3]. None of the physicians sampled benefitted from any one-health-related seminar [Table 4]. Most physicians needed to be made aware of the objectives of the ZDU [Table 5].
Socio-demographic characteristics of OHCs
| Characteristics, n = 142 | Frequency (n) | Percentage (%) |
| Age group in years | ||
| < 45 | 100 | 70.4 |
| 45+ | 42 | 29.6 |
| Range 24-58 | ||
| Mean ± sd 39.7 ± 9.5 | ||
| Gender | ||
| Male | 83 | 58.4 |
| Female | 59 | 41.6 |
| Sector | ||
| Human Health | 119 | 83.8 |
| Veterinary | 20 | 14.1 |
| Wildlife | 3 | 2.1 |
| Professional background | ||
| Physician | 55 | 38.7 |
| Public health officer | 64 | 45.1 |
| Veterinarian | 6 | 4.2 |
| Veterinary paraprofessional | 14 | 9.9 |
| Wildlife paraprofessional | 1 | 0.7 |
| Wildlife ecologist | 2 | 1.4 |
| Highest level of education | ||
| Certificate | 11 | 7.7 |
| Diploma | 40 | 28.2 |
| Bachelor | 77 | 54.2 |
| Masters | 14 | 9.9 |
Distribution of respondents according to awareness of the existence of a Zoonotic Disease Unit in Kenya
| Professional background | Awareness of the Zoonotic Disease Unit in Kenya | |
| Yes n (%) | No n (%) | |
| Physician | 12 (21.82) | 43 (78.18) |
| Public health officer | 35 (54.69) | 29 (45.31) |
| Veterinarian | 6 (100.0) | 0 (0.0) |
| Veterinary paraprofessional | 9 (64.29) | 5 (35.71) |
| Wildlife paraprofessional | 1 (100.0) | 0 (0.0) |
| Ecologist | 1 (50.0) | 1 (50.0) |
| Total | 64 (45.07) | 78 (54.93) |
Attendance of any One Health-related course by the OHCs
| Professional background | Course attended | ||||
| None n (%) | Environmental health (Meat inspection) n (%) | Disease surveillance n (%) | Animal welfare n (%) | Bio-surveillance of zoonoses n (%) | |
| Physician | 55 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Public health officer | 58 (90.6) | 0 (0.0) | 6 (9.4) | 0 (0.0) | 0 (0.0) |
| Veterinarian | 4 (66.7) | 0 (0.0) | 2 (33.3) | 0 (0.0) | 0 (0.0) |
| Veterinary paraprofessional | 2 (14.3) | 12 (85.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Wildlife paraprofessional | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) |
| Ecologist | 1 (50.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) |
| Total | 120 (84.5) | 12 (8.5) | 8 (5.6) | 1 (0.7) | 1 (0.7) |
Attendance of One Health-related seminar by OHCs
| Professional background | Seminar attended | |||||||
| None n (%) | AMR n (%) | Zoonoses n (%) | Climate change n (%) | COVID-19 disease n (%) | Response and surveillance for rabies n (%) | Food safety n (%) | Disease surveillance n (%) | |
| Physician | 54 (98.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.8) |
| PHO | 18 (28.1) | 0 (0.0) | 4 (6.3) | 0 (0.0) | 7 (10.9) | 1 (1.6) | 1 (1.6) | 33 (51.6) |
| Veterinarian | 0(0.0) | 6 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| VPP | 7 (50.0) | 0 (0.0) | 0 (0.0) | 1 (7.1) | 0 (0.0) | 0 (0.0) | 6 (42.9) | 0 (0.0) |
| WPP | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Ecologist | 1 (50.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | (0.0) | 1 (50.0) |
| Total | 81 (57.0) | 6 (4.2) | 4 (2.8) | 1 (0.7) | 7 (4.9) | 1 (0.7) | 7 (4.9) | 35 (24.6) |
Respondents’ knowledge of the objectives of the Zoonotic Disease Unit of Kenya
| Professional background | Objectives of the Zoonotic Disease Unit | |||
| Did not know n (%) | Listed one objective n (%) | Listed two objectives n (%) | Listed three objectives n (%) | |
| Physician | 42 (76.8) | 8 (14.3) | 5 (8.9) | 0 (0.0) |
| PHO | 29 (45.3) | 29 (45.3) | 6 (9.4) | 0 (0.0) |
| Veterinarian | 0 (0.0) | 0 (0.0) | 5 (83.3) | 1 (16.7) |
| VPP | 5 (35.7) | 6 (42.9) | 3 (21.4) | 0 (0.0) |
| WPP | 0 (0.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) |
| Ecologist | 1 (50.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) |
| Total | 77 (54.5) | 44 (30.8) | 20 (14.0) | 1 (0.7) |
The proportion of OH practitioners collaborating to control zoonoses in Kisumu County was 51.4%. Most instances of collaboration were initiated by the human health sector [Table 6].
Extent of intersectoral collaboration among One Health partners
| Collaboration by sector | Responses | ||
| n | Proportion | 95%CI | |
| Health workers collaborating with veterinarians | 70 | 47.9% | 41.1, 57.6 |
| Health workers collaborating with wildlife/ecosystem experts | 2 | 1.4% | 0.3, 5.5 |
| Veterinarians collaborating with health workers | 65 | 44.5% | 37.7, 54.1 |
| Veterinarians collaborating with wildlife/ecosystem experts | 3 | 2.1% | 0.7, 6.4 |
| Wildlife/ecosystem experts collaborating with health workers | 3 | 2.1% | 0.7, 6.4 |
| Wildlife/ecosystem experts collaborating with veterinarians | 3 | 2.1% | 0.7, 6.4 |
Nature of collaboration among OH practitioners
Most (86.3%) of the OH partners participating in the collaboration notified their counterparts whenever a zoonosis was encountered, with public health professionals initiating most instances of the partnership [Table 7]. Sharing of surveillance information, conducting joint sensitizations/advocacy, joint surveillance, sharing of vehicles during vaccinations, and collaboration through professional associations were also frequently reported (53.4%, 30.1%, 27.4%, and 20.5%, respectively). Veterinarians, veterinary paraprofessionals, wildlife paraprofessionals, and ecologists did not share refrigerators or vehicles during vaccination campaigns. Joint surveillance was only conducted by physicians, public health officers, and ecologists [Table 7].
Nature of collaboration among OH partners for control of zoonoses
Nature of collaboration | |||||||
| Physician n (%) | PHO n (%) | Veterinarian n (%) | VPP n (%) | WPP n (%) | Ecologist n (%) | Total n (%) | |
| Sharing refrigerators | 0 (0.0) | 1(0.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.6) |
| Sharing vehicles during vaccination | 3 (1.7) | 4 (2.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 7 (4.1) |
| Sharing surveillance information | 9 (5.2) | 20 (11.6) | 3 (1.7) | 5 (2.9) | 0 (0.0) | 2(1.2) | 39 (22.7) |
| Conducting surveillance together | 6 (3.5) | 13 (7.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.1) | 20 (11.6) |
| Conducting joint sensitizations/advocacy | 4 (2.3) | 14 (8.1) | 0 (0.0) | 1 (0.6) | 1 (0.6) | 2 (1.2) | 22 (12.8) |
| Notifying other sectors when a zoonosis is encountered | 11 (6.4) | 29 (16.9) | 6 (3.5) | 14 (8.1) | 1 (0.6) | 2 (1.2) | 63 (36.6) |
| Notifying other sectors when training opportunities arise | 0 (0) | 4 (2.3) | 0 (0,0) | 1 (0.9) | 0 (0.0) | 0 (0.0) | 5 (2.9) |
| Collaboration through professional associations | 7 (4.1) | 2 (1.2) | 1 (0.6) | 3 (1.7) | 1 (0.6) | 1 (0.6) | 15 (8.7) |
| Total | 40 (23.3) | 87 (50.6) | 10 (5.8) | 24 (14) | 3 (1.7) | 8 (4.7) | 172(100) |
Factors that prompted the collaboration
Medical officers, veterinary paraprofessionals, and wildlife paraprofessionals were prompted to collaborate by the need for particular expertise outside their sector. Veterinary officers and public health officers were prompted to collaborate by the desire to promote One Health [Table 8].
Factors that Prompted OH collaboration
| Cues to collaboration | Professional background | ||||||
| Physician n (%) | PHO n (%) | Veterinarian n (%) | VPP n (%) | WPP n (%) | Ecologist n (%) | Total n (%) | |
| Adequate transport | 0 (0.0) | 5 (2.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (2.7) |
| Need for that expertise | 14 (7.6) | 27 (14.6) | 4 (2.2) | 13 (7.0) | 1 (0.5) | 2 (1.1) | 61 (33) |
| Sufficient funding | 0 (0.0) | 1 (0.5) | 1 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (1.1) |
| Need to promote One Health | 8 (4.3) | 30 (16.2) | 6 (3.3) | 12 (6.5) | 1 (0.5) | 2 (1.1) | 59 (31.9) |
| Government policy | 13 (7.0) | 27 (14.6) | 4 (2.2) | 13 (7.0) | 0 (0.0) | 1 (0.1) | 58 (31.4) |
Factors that affect collaboration among OH practitioners in the control of zoonoses
Most health workers and veterinarians cited insufficient funding (P = 0.000), lack of communication (P = 0.000), lack of transport facilities (P = 0.000), lack of interest in zoonoses at work and during training (P = 0.000), and difference in emphasis on zoonoses (P = 0.002) as the significant factors affecting OH collaboration [Table 9].
Factors that affected collaboration among OH practitioners
| Factors | Responses n (%) | Chi-Square | df | P-value |
| Lack of communication | 120 (13.7) | 24.429 | 5 | 0.000 |
| Lack of transport facilities | 101(11.5) | 24.539 | 5 | 0.000 |
| Lack of interest in zoonoses at work and during training | 93 (10.6) | 24.267 | 5 | 0.000 |
| Insufficient funding | 123(14.1) | 33.803 | 5 | 0.000 |
| Budgetary separation of health and veterinary departments | 80 (9.1) | 5.102 | 5 | 0.404 |
| Differences in emphasis on | 102 (11.7) | 19.565 | 5 | 0.002 |
| Lack of intersectoral trust | 60 (6.9) | 6.629 | 5 | 0.250 |
| Weak public health infrastructure | 122 (13.9) | 5.592 | 5 | 0.348 |
| The institutional separation of health and veterinary departments | 74 (8.5) | 14.810 | 5 | 0.011 |
When requested to comment on the factors affecting multisectoral collaboration, more specifically, respondents indicated that communication enhances cooperation and facilitates engagement at departmental levels and that lack of it may frustrate collaborators’ efforts. Transport was needed to strengthen responses where collaboration was required. While funding was necessary to support One Health operations such as training, sensitization meetings, and advocacy for OH approaches [Table 10].
How factors affected OH collaboration
| Factor | Effect | Frequency | Percent |
| Lack of communication | It does not affect One Health | 22 | 15.5 |
| Cooperation is not enhanced | 69 | 48.6 | |
| Uncertain | 3 | 2.1 | |
| This leads to disjointed efforts | 5 | 3.5 | |
| Facilitates engagement at departmental levels | 43 | 30.3 | |
| Lack of transport | Does not hinder collaboration | 26 | 18.3 |
| Responses are not enhanced where collaboration is needed | 101 | 71.1 | |
| Uncertain | 15 | 10.6 | |
| Lack of interest in zoonoses at work and during training | Does not hinder collaboration | 22 | 15.5 |
| Some health workers do not understand the impact of zoonoses | 13 | 9.2 | |
| Uncertain | 27 | 19.0 | |
| Interest should drive One Health | 15 | 10.6 | |
| Departments promote their core mandates only | 12 | 8.5 | |
| Concern for veterinarians | 26 | 18.3 | |
| It is only a public health concern during outbreaks | 11 | 7.7 | |
| Zoonoses are not common in urban settings | 10 | 7.0 | |
| Capacity building is inadequate | 6 | 4.2 | |
| Insufficient funding | Does not hinder collaboration | 7 | 4.9 |
| Funding can support One Health operations | 76 | 53.5 | |
| Limits research on emerging and infectious diseases | 3 | 2.1 | |
| Uncertain | 12 | 8.5 | |
| Limit development of One Health Infrastructure | 2 | 1.4 | |
| Training opportunities not supported | 26 | 18.3 | |
| Advocacy not Supported | 16 | 11.3 | |
| Lack of emphasis on zoonoses at work and during training | Does not hinder collaboration | 12 | 8.5 |
| Hampers multisectoral communication | 22 | 15.5 | |
| Uncertain | 28 | 19.7 | |
| Need to deliver on core mandates | 25 | 17.6 | |
| No clear policy to guide collaboration | 18 | 12.7 | |
| Specialization increases focus on one area | 31 | 21.8 | |
| Insufficient staff | 6 | 4.2 | |
| Lack of intersectoral trust | Does not hinder collaboration | 38 | 26.8 |
| Hampers communication | 17 | 12.0 | |
| Uncertain | 44 | 31.0 | |
| Affects coordination | 21 | 14.8 | |
| Some departments feel superior to others | 14 | 9.9 | |
| Blame game over perceived failure/inaction of a department | 8 | 5.6 |
DISCUSSION
The extent of collaboration among OH practitioners
In this study, most collaboration was between the sectors responsible for health and livestock and primarily driven by the efforts of PHOs, unlike in Tanzania, where the animal health sector was instrumental[20]. Collaboration between the wildlife and health sectors needed improvement due to the low staffing level that restricted their focus on ecosystem conservation. The better performance of the human health sector over the animal health sector was attributed to the low staffing levels in the latter due to increased workload while concentrating on the perceived core mandates, which left little opportunity for interactions with their OH partners. Understaffing was common in the veterinary and wildlife sectors. Indeed, only three wildlife experts were deployed across the study area, with one wildlife veterinarian serving Kisumu County from the Nairobi office.
Although public and veterinary services are devolved functions in Kenya, the national government retained policy formulation. However, since a county-level OH coordinating unit was not in place, the OH policy needed to be revised regarding practical guidance, promotion, and sustenance of multisectoral collaboration. This observation compares well with a Tanzanian study where a lack of policy statements contributed to the insufficient collaboration between physicians and veterinarians[20]. This inadequate collaboration should concern disease control experts since most zoonotic disease pathogens originate from the wildlife sector[21]. Medical officers (MOs) make critical decisions regarding disease control in hospitals and populations. For that reason, the low awareness of the existence of the ZDU and its objectives is a source of concern but explains the low level of cross-sector collaboration.
The level of post-basic training for the OHC could have been higher, as shown by the slow uptake of courses and seminars. The few staff who benefited from the Kenya Field and Epidemiology Training program needed to be adequately deployed to drive the OH agenda. Indeed, only some of the MOs sampled attended any OH course, and fewer participated in an OH-related seminar. However, much focus on curative services, though necessitated by staffing regime and the increasing number of patients, in addition to specialization, significantly reduced opportunities for collaboration.
Nature of collaboration among OH practitioners
Whereas a policy on OH existed at the national government level, there appeared to be some lethargy in its implementation, indicating either inadequacy of the document or lack of motivation. Partners were prompted to collaborate by the need for expertise outside their work sector. However, as noted elsewhere, the need for knowledge in disease detection and response, targeted surveillance and notification systems, joint meetings, and activities provided cues for partners to collaborate[22]. Due to their role as extension agents of the human health sector and appreciable staffing inventory, PHOs undertook most of the daily One Health activities[20].
Sharing surveillance information and other forms of notification on suspected zoonosis was common in collaboration among partners. Even though the wildlife sector is widely regarded as a source of zoonotic infections, human and animal health engagement was limited. However, with its smaller workforce, the wildlife sector shared information across all sectors. Collaboration through joint activities should have provided an opportunity for partnership but needed to be improved due to resource constraints and low staff levels in the animal and wildlife sectors.
Factors affecting OH collaboration
As observed elsewhere, some factors influencing OH collaboration are sector-specific[23]. Insufficient funding had the most influence on the practice of OH since funds are required to support one health operations, such as training practitioners through seminars or short courses, and acquisition of critical infrastructures such as vehicles, offices, communication systems, and other materials[20,24,25]. OH collaboration would ideally succeed with an adequately trained, appropriately deployed, motivated, and properly equipped workforce. A multisectoral collaboration, as part and parcel of the health system, requires clearly defined unifying OH effort, champions and partners, clear policy direction, and allocation of adequate resources to expand its capacity for better preparedness and resilience[25,26]. Such kind of infrastructure was lacking.
A communication system is fundamental to the success of any OH approach since it drives peer engagement and enhances rapid community education about disease outbreaks and management[27]. Communication across the collaborating sectors allows sharing of surveillance data and planning. According to this study, communication among collaborating partners can enhance knowledge integration and cooperation through engagement at different departmental levels, as observed elsewhere[25,28]. Communication failure was mainly due to inadequate policy, as in Tanzania, where such a policy needed to be improved[20].
Placing much focus on perceived critical departmental objectives could have improved collaboration, such that some veterinarians should have considered veterinary services as part of human health. Human health experts concentrated on curative services, ignoring the potential of a preventive approach to zoonoses[24]. Where curative health services are prioritized, the need to consult with collaborating partners remains the same. Preventive and control measures need to start in the wildlife phase, followed by the livestock sector, which is a buffer between the wildlife sector, which is regarded as the source of most zoonotic pathogens, and the human hosts[24,29]. In this study, some human health experts wrongly assumed that zoonotic diseases were the domain of veterinarians. Some OH partners did not appreciate the full impact of zoonoses, while for some, it was only an issue outside the urban settings. This observation is attributed to continued specialization and inadequate post-basic course training, including a need for opportunities for acquiring new knowledge on zoonoses[27,30].
In conclusion, multisectoral collaboration for OH needed to be improved due to a deficient OH policy at the Kisumu County level. The proportion of human health experts collaborating for OH was higher than their animal health and wildlife counterparts. Conducting joint sensitizations and notification of partners whenever a zoonosis was encountered were the preferred collaboration methods. The main barriers to multisectoral collaboration were the need for more funding, inadequate communication, lack of transport facilities, and low interest in zoonoses at work and during training. The need for particular expertise, the desire to promote OH, and the requirement to mainstream OH as a departmental policy prompted partners to collaborate.
The study recommends reviewing the OH policy under the leadership of the Zoonotic Disease Unit to enhance guidance and sustainability at the county level. The formation of a well-resourced county-level coordination unit by Kisumu County public service is critical to driving the OH agenda. To enhance interest in the OH approach, there is a need to entrench it in the syllabus of all health-related courses by training institutions. Setting up an automated real-time alert system that enhances data collection, processing, and dissemination can address the lack of communication. The study recommends further study on the low interest in one health among physicians despite their critical role in the approach’s success.
DECLARATIONS
AcknowledgmentsThe authors thank the respondents for giving their precious time to fill in the questionnaire used for data collection.
Authors’ contributionsMade substantial contributions to the conception and design of the study and performed data analysis and interpretation: Onyango ND
Provided administrative, technical, and material support: Onguru DO, Atieno OA
Availability of data and materialsData will be available upon request to the corresponding author.
Financial support and sponsorshipNone.
Conflicts of interestsAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateEthical approval was obtained from the Ethics Committee of Jaramogi Oginga Odinga Teaching and Referral Hospital, Kisumu (No. IERC/JOOTRH/347/20), and written consent was given by the respondents.
Consent for publicationNot applicable.
Copyright© The Authors 2023.
REFERENCES
1. OIE. Tripartite and UNEP support OHHLEP’s definition of “One Health”. Available from: https://www.oie.int/en/tripartite-and-unep-support-ohhleps-definition-of-one-health/. [Last accessed on 26 Apr 2023].
2. Hamilton K, Nutter F, Olson D, Steele J. USAID RESPOND project's global one health core competencies and one health modules. Annals of Global Health 2018;81:150-1.
3. National Center for Emerging and Zoonotic Infectious Diseases (NCEZID). Available from: https://www.cdc.gov/ncezid/index.html. [Last accessed on 26 Apr 2023].
4. WHO. One Health. Available from: https://www.who.int/news-room/q-a-detail/one-health. [Last accessed on 26 Apr 2023].
5. WHO. Asia Pacific Strategy for emerging diseases:2010. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3729053/. [Last accessed on 26 Apr 2023].
6. Bloom DE, Black S, Rappuoli R. Emerging infectious diseases: A proactive approach. Proc Natl Acad Sci USA 2017;114:4055-9.
7. Zowalaty ME, Järhult JD. From SARS to COVID-19: A previously unknown SARS- related coronavirus (SARS-CoV-2) of pandemic potential infecting humans - Call for a One Health approach. One Health 2020;9:100124.
8. Morens DM, Fauci AS. Emerging infectious diseases: threats to human health and global stability. PLoS Pathog 2013;9:e1003467.
9. Gebreyes WA, Dupouy-Camet J, Newport MJ, et al. The global one health paradigm: challenges and opportunities for tackling infectious diseases at the human, animal, and environment interface in low-resource settings. PLoS Negl Trop Dis 2014;8:e3257.
10. Munyua PM, Njenga MK, Osoro EM, et al. Successes and challenges of the One Health approach in Kenya over the last decade. BMC Public Health 2019;19:465.
11. FAO, OIE W. High-Level Technical Meeting to Address Health Risks at the Human-Animal- Ecosystems Interfaces. Available from: https://apps.who.int/iris/handle/10665/78100. [Last accessed on 26 Apr 2023].
12. World Bank. People, Pathogens and Our Planet, Volume 1: Towards a One Health Approach for Controlling Zoonotic Diseases, Available from: https://documents.worldbank.org/en/publication/documents-reports/documentdetail/214701468338937565/volume-one-towards-a-one-health-approach-for-controlling-zoonotic-diseases. [Last accessed on 26 Apr 2023].
13. Okello AL, Bardosh K, Smith J, Welburn SC. One Health: past successes and future challenges in three African contexts. PLoS Negl Trop Dis 2014;8:e2884.
14. Sikkema R, Koopmans M. One Health training and research activities in Western Europe. Infect Ecol Epidemiol 2016;6:33703.
15. Mbabu M, Njeru I, File S, et al. Establishing a One Health office in Kenya. Pan Afr Med J 2014;19:106.
16. Rwego IB, Babalobi OO, Musotsi P, et al. One Health capacity building in sub-Saharan Africa. Infect Ecol Epidemiol 2016;6:34032.
17. . Kenya National Bureau of Statistics. County Government of Kisumu. Kisumu livestock statistics and products 2022. Kisumu; 2022 Mar. Available from: https://www.knbs.or.ke/wp-content/uploads/2022/05/2022-Economic-Survey1.pdf. [Last accessed on 26 Apr 2023]
18. ZDU. One Health Strategic Plan for the Prevention and Control of Zoonotic Diseases in Kenya (2021-2025). Available from: https://www.health.go.ke/wp-content/uploads/2022/04/One-Health-Strategic-Plan-_Kenya_2021-2025.pdf. [Last accessed on 26 Apr 2023].
19. Cochran WG. Sampling techniques, 3rd Edition. Available from: https://www.wiley.com/en-ke/Sampling+Techniques%2C+3rd+Edition-p-9780471162407. [Last accessed on 26 Apr 2023].
20. Kayunze KA, Kiwara A, Lyamuya E, et al. Practice of One Health approaches: bridges and barriers in Tanzania. Onderstepoort J Vet Res 2014;81:E1-8.
21. Zheng Z, Lu Y, Short KR, Lu J. One health insights to prevent the next HxNy viral outbreak: learning from the epidemiology of H7N9. BMC Infect Dis 2019;19:138.
22. Adamson S, Marich A, Roth I. One Health in NSW: coordination of human and animal health sector management of zoonoses of public health significance. N S W Public Health Bull 2011;22:105-12.
23. Dos S Ribeiro C, van de Burgwal LHM, Regeer BJ. Overcoming challenges for designing and implementing the One Health approach: A systematic review of the literature. One Health 2019;7:100085.
24. Courtenay M, Sweeney J, Zielinska P, Brown Blake S, La Ragione R. One Health: An opportunity for an interprofessional approach to healthcare. J Interprof Care 2015;29(6):641-2.
25. OIE. OIE, PVS Gap Analysis - Nepal. 2011. Available from: https://extranet.who.int/sph/country/nepal. [Last accessed on 26 Apr 2023].
26. Ruscio BA, Brubaker M, Glasser J, Hueston W, Hennessy TW. One Health - a strategy for resilience in a changing arctic. Int J Circumpolar Health 2015;74:27913.
27. Mwangi W, de Figueiredo P, Criscitiello MF. One Health: Addressing Global Challenges at the Nexus of Human, Animal, and Environmental Health. PLoS Pathog 2016;12:e1005731.
28. Hitziger M, Esposito R, Canali M, Aragrande M, Häsler B, Rüegg SR. Knowledge integration in One Health policy formulation, implementation and evaluation. Bull World Health Organ 2018;96:211-8.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Onyango ND, Onguru DO, Atieno OA. Effectiveness of multisectoral collaboration in implementation of One Health Approach for control of zoonoses in Kisumu, Kenya. One Health Implement Res 2023;3:30-41. http://dx.doi.org/10.20517/ohir.2022.29
AMA Style
Onyango ND, Onguru DO, Atieno OA. Effectiveness of multisectoral collaboration in implementation of One Health Approach for control of zoonoses in Kisumu, Kenya. One Health & Implementation Research. 2023; 3(2): 30-41. http://dx.doi.org/10.20517/ohir.2022.29
Chicago/Turabian Style
Onyango, Nobert D., Dan O. Onguru, Ochung’ Angeline Atieno. 2023. "Effectiveness of multisectoral collaboration in implementation of One Health Approach for control of zoonoses in Kisumu, Kenya" One Health & Implementation Research. 3, no.2: 30-41. http://dx.doi.org/10.20517/ohir.2022.29
ACS Style
Onyango, ND.; Onguru DO.; Atieno OA. Effectiveness of multisectoral collaboration in implementation of One Health Approach for control of zoonoses in Kisumu, Kenya. One. Health Implement. Res. 2023, 3, 30-41. http://dx.doi.org/10.20517/ohir.2022.29
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 14 clicks
Cite This Article 14 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.